Notice: Function Elementor\Controls_Manager::add_control_to_stack was called incorrectly. Cannot redeclare control with same name "eael_image_masking_upload_pro_message". Please see Debugging in WordPress for more information. (This message was added in version 1.0.0.) in /data/web/e44470/html/apps/wordpress-92643/wp-includes/functions.php on line 6121
Notice: Function Elementor\Controls_Manager::add_control_to_stack was called incorrectly. Cannot redeclare control with same name "eael_image_masking_upload_pro_message". Please see Debugging in WordPress for more information. (This message was added in version 1.0.0.) in /data/web/e44470/html/apps/wordpress-92643/wp-includes/functions.php on line 6121
Notice: Function Elementor\Controls_Manager::add_control_to_stack was called incorrectly. Cannot redeclare control with same name "eael_image_masking_upload_pro_message". Please see Debugging in WordPress for more information. (This message was added in version 1.0.0.) in /data/web/e44470/html/apps/wordpress-92643/wp-includes/functions.php on line 6121
Rubber Band Treatment of Haemorrhoidal Prolaps
Notice: Function Elementor\Controls_Manager::add_control_to_stack was called incorrectly. Cannot redeclare control with same name "eael_image_masking_upload_pro_message". Please see Debugging in WordPress for more information. (This message was added in version 1.0.0.) in /data/web/e44470/html/apps/wordpress-92643/wp-includes/functions.php on line 6121
Office treatments for haemorrhoidal prolaps consist of various methods short of surgical intervention. The most commonly used methods today are rubber band ligation, infrared photocoagulation, biclamp-coagulation, sclerotherapy and cryotherapy. Cryotherapy is rarely used today.
Barron originally described the most common method currently in use for the outpatient treatment for haemorrhoids in 1963. Rubber band ligation is commonly recommended for individuals suffering from Grade I or Grade II haemorrhoids and, in some circumstances, Grade III haemorrhoids.
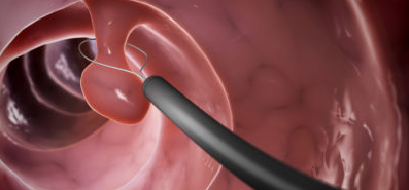
In preparation, patients are asked to take 1 or 2 CO2 laxative suppositories. After anal examination, a slightly larger anoscope is inserted and the haemorrhoid to be banded is identified (generally the largest haemorrhoid is banded first) and thru suction ligated at its basis. Once this has been accomplished, the patient is asked if he or she feels any pain. Pain indicates somatic, not autonomic, innervations of the mucosa at that level. At this point, the band should be applied. If the patient does not experience any pain or discomfort then the rubber band is applied by depressing the trigger on the haemorrhoid ligator. This treatment is only applicable, of course, to asensate, internal haemorrhoids above the dentate line. Some individuals prefer to band all three haemorrhoids at one setting, however this may results in significant discomfort. It is my practice to band one haemorrhoid at the first setting. If the patient tolerates this well, then at the second setting (three weeks later) the second and third haemorrhoids will be banded. If the first banding, however, has been difficult, then the remaining haemorrhoids will be banded one at a time.
Relapse rates following banding in our experience found 23% of patients required repeat banding over 5 years and 32% at 10 years, and felt haemorrhoid banding to be a durable procedure.
Haemorrhoidal banding is successful in two thirds to three quarters of all individuals with first and second degree haemorrhoids. Most individuals respond to banding of the three common haemorrhoidal bundles although this may need to be repeated in the future. Rarely individuals fail to respond whatsoever or cannot tolerate banding and may require formal haemorrhoidectomy.
Recently our group for haemorrhoid banding has developed a new device. An anoscope equipped with a Doppler identifies specifically the haemorrhoidal artery feeding the pile and with a side-view suction ligator is proven alternative to traditional banding methods. The anoscope is inserted and directed at the appropriate haemorrhoid and suction applied.
Complications of haemorrhoid banding are very seldom and include bleeding, pain, thrombosis and in very rare cases life threatening perineal sepsis. Bleeding generally occurs immediately after banding or 7-10 days later when the band falls off. This is a rare occurrence but occasionally operative intervention is required to control persistent haemorrhage. A dull persistent ache is common for the first one to two days following banding. Significant anal pain is rare but is often secondary to a rubber band placed too close to the dentate line. If the pain is experienced immediately following the banding, then the rubber band can be removed with a beaver blade, although this is a difficult procedure. If the patient develops pain later on then this is generally treated with sit-baths, analgesics and occasionally antispasmodics. It is important to avoid constipation during this period as well. Rarely, haemorrhoid banding can result in thrombosis of internal and external haemorrhoids resulting in significant pain. There have been several anecdotal cases of life threatening perianal sepsis following haemorrhoid banding.(15) Patients are therefore asked to watch for the cardinal signs of this phenomenon which would be significant pain, fever, and difficulty urinating. Although there is only anecdotal evidence, some authors recommend avoiding haemorrhoidal banding in individuals with immune compromised states because of the potential risk of perianal sepsis.
Prospectively studied complications in 1600 patients undergoing haemorrhoid banding, minor complications developed in 4.6% of patients including pain, band slippage, mucosal ulcer, and anal thrombosis. Hospitalization for major complications was necessary in less than 1.5%, and included haemorrhage, severe pain and urinary retention.
After Treatment
Symptoms
You may feel mild to moderate pain, a dull ache, or essentially nothing for the first 36 to 48 hours. A sense of urgency to have a bowel movement is normal after these treatments. If discomfort is mild, take over-the-counter medications such as Ibuprofen or Diclofenac. Do not take aspirin or products containing aspirin since they may promote bleeding. If your pain is more severe, you will be given a prescription for pain medicine. Taking warm baths with Kamillosan for 15 to 20 minutes will help relieve your discomfort.
Generally it takes two to four treatments three to six weeks apart to get rid of all the prolapsing mucous. Usually only one area, or occasionally two, is treated at a time. Remember that bleeding and prolapse will probably persist until all the haemorrhoids and prolapsing tissue have been treated.
Diet
After your treatment, it is important to keep your bowel movements soft and regular. Eat foods high in fibre and drink lots of water (6-8 glasses a day). Continue the fibre supplement recommended by your doctor. Caffeine contributes to constipation so limit your consumption of coffee, tea, colas, and chocolate. Electrolyte substitution like Magnosolv Granulat may help while rending your stool softer
Activity
You may continue your normal physical activities. You will be able to drive your car immediately, walk up stairs, and do normal exercise.
Causes for Concern: Call the doctor if you have any of the following problems:
a) Pain that does not gradually lessen in three days,
b) Increasing pain several days after treatment,
c) Tender swelling in the anal area, fever or chills, difficulty urinating, drainage of pus from the rectum
d) Increased bleeding (more than one cupful)
e) Three to four large bloody bowel movements within three hours
f) Severe constipation (no bowel movement for three days)
g) Diarrhoea (more than three watery stools within 24 hours)
In an emergency try to contact us for advice before you go to the hospital. A telephone call may save you a lot of time, discomfort and expense.
Speciality

Venous Disease Centre
Chronic venous insufficiency or CVI is a medical condition where the veins cannot pump enough blood back to the heart. It is sometimes referred to as an "impaired musculovenous pump", this is due to damaged or "incompetent" valves. Are your veins pumping out, your skin discoloured, legs swelling, feeling heavy or crampy: if your legs feel uncomfortable, get a vascular check-up. It does not hurt.

Centre for Proctology
The Clinic together with Consultants from the Vienna University Clinic offers advanced diagnostic and therapeutic services including robotic colorectal surgery for disorders of the colon, rectum, anus and pelvic floor within a friendly and reassuring environment. The Rapid Access Proctology Clinic reduces waiting time and improve public and professional awareness of the need for early detection and treatment of colorectal lesions

Endoscopy Centre
The Endoscopy Centre performs a comprehensive range of endoscopic procedures that allow both diagnosis and treatment of gastrointestinal disorders, such as peptic ulcers, polyps, inflammation and tumors. It is professionally committed to ensuring that your experience with us is relaxed and worry-free, from consultation through recovery. To assist us in achieving a mutual satisfactory procedure, we ask that you read our guidelines.
Treatments
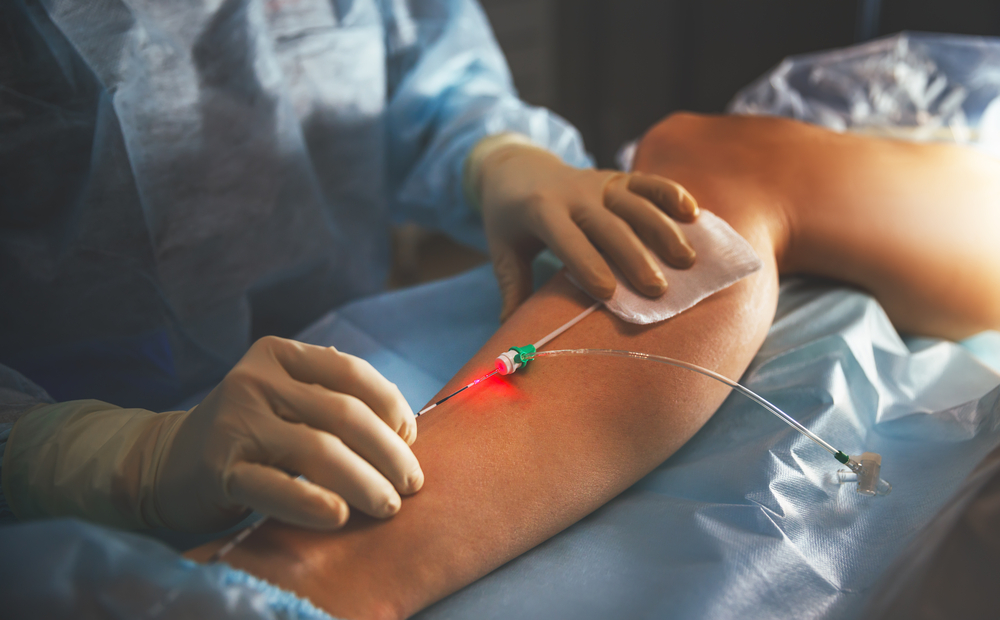

Endovenous Laser Treatment
Endovenous laser treatment is a procedure to treat larger varicose veins in the legs. A laser fibre is passed through a thin tube (catheter) into the vein. While doing this, the doctor watches the vein on a duplex ultrasound screen. Laser is less painful than vein ligation and stripping, and it has a shorter recovery time. Only local diluted anaesthesia is needed with mild sedation for this laser treatment.
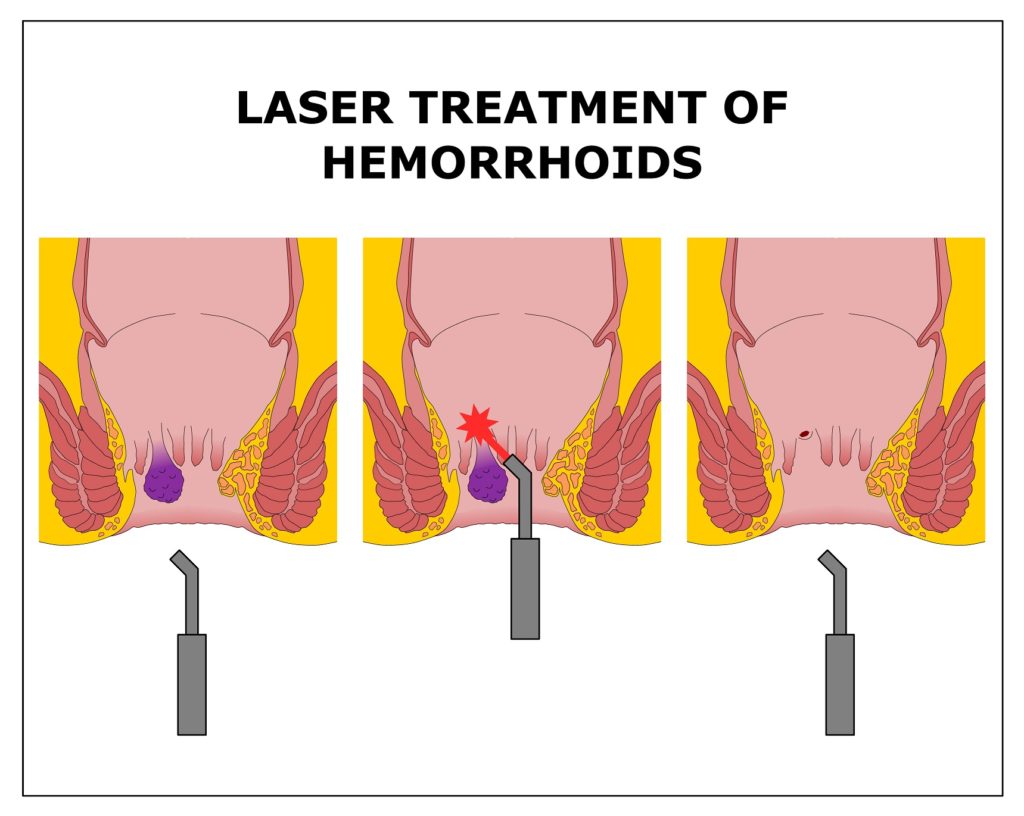

Laser-assisted Haemorrhoidectomy
The Clinic offers the newest laser technology for surgical treatment assisted with Duplex sonography for internal haemorrhoids. The procedure permits a smoother, less painful and faster recovery. The affected area is treated with pinpoited laser energy to the affected haemorrhoid and the problem is solved within a few minutes. Patients can resume their normal lives immediately after surgery.
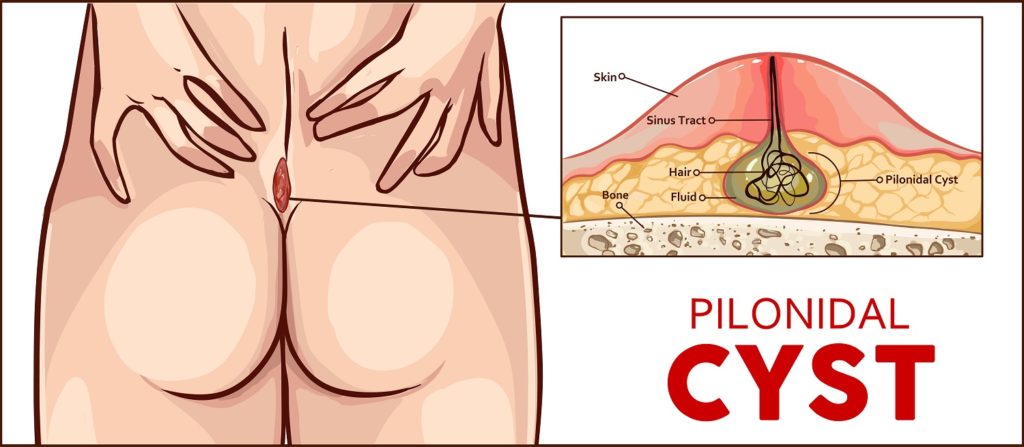

Pit Picking and Laser-assisted sinusectomy
The Endoscopy Center is professionally committed to ensuring that your experience with us is relaxed and worry-free, from consultation through recovery. To assist us, we ask that you read and comply with all our guidelines. Endoscopic laser-assisted sinusectomy shows a low recurrence rate and marsupilisation of the wound a prompt healing. Following this procedure patients can return to work shortly afterwards. Mild discomfort while the procedure is performed in local analgesia is corrected with light sedation and with over the counter pain killers in the immediate postoperative period.
Where to find us

The Sievering Clinic
The Sievering Clinic is situated in the heart of the private medical services in Vienna with Rudolfiner Hospital just across the street. It is a surgical outpatient clinic offering state-of-art diagnosis and treatments for the fields of phlebology (diagnosis and treatment of vascular disease), proctology (diseases of the rectum) and gastrointestinal diseases.



City Clinic in Heiligenkreuzerhof
You can also visit us at our private clinic in the centre of the city. Heiligenkreuzerhof offers great access just a few minutes from St Stephen and sufficient parking area at Schwedenplatz. Walking distance from the U1 Stephanplatz and U1 U4 Schwedenplatz
Appointments
To request an appointment at Dr Bull’s Clinic fill out the Online form and click “Send Form.” We will contact you only if the scheduled appointment has to be postponed or amended . If you do not feel comfortable with this method just call 01 328 8777 or 01 512 2458 we will be there for you.
Please note: This request form is not intended as a tool for reporting a medical emergency or medical problem. It will not go to a physician and is only monitored during normal business hours. If you have critical or timely information, please contact a physician directly. If you have a medical emergency, please call 112.
Patient Information
We provide outpatient care for the patients referred by their general practitioner (GP) with all types of problems. The staff in the clinic understand that it may take courage to attend, especially when you are feeling worried or anxious. Our aim is that you leave the clinic as reassured as possible. We want your visit to be a friendly and helpfull experience.
To make your admission process to the Clinic as smooth and stress-free as possible please review your patient information guide.