This guide is for patients who are going to have colonoscopy. It answers some of the most commonly asked questions. Please don’t hesitate to ask your doctor or nurse for more information.
What is a Colonoscopy?
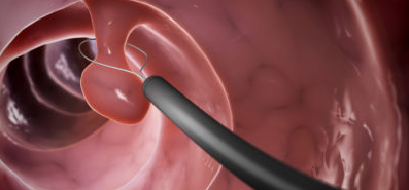
A colonoscopy is an examination of the lining of the colon with a lighted, flexible tube about the thickness of your finger. The doctor will insert the tube through your rectum, then up through your colon to check for abnormalities. If necessary, an instrument can be passed through the tube to take a small piece of tissue (a biopsy) for examination in the lab. Biopsies are done for many reasons and do not necessarily imply cancer. Often during this process of diagnosis, your doctor may perform other minor procedures, such as polyp removal.
Preparing for your test
Please contact your primary care physician or insurance company if prior referral is needed.
The procedure will take about 45 minutes, but expect the visit to the Medical Procedures Unit to last about four (4) hours to allow for preparation and recovery.
ONE WEEK (SEVEN DAYS) BEFORE YOUR TEST:
Arrange for a responsible person to accompany you to your appointment.
Do not take aspirin for one (1) week prior to your appointment. A few of these products include:
- Aspirin
- Anacin
- Ascripton
- Bufferin
- Ecotrin
- ThromboAss.
Do not take Plavix or non-steroidal anti-inflammatory drugs for two (2) days prior to your appointment as all of these drugs may increase bleeding. A few of these products are:
- Advil
- Aleve
- Anaprox
- Motrin
- Naprosyn
- Nuprin
Do not take iron or herbal supplements for one week prior to your procedure.
You may continue Celebrex. If you are unsure about the medications you are taking, ask your nurse or doctor.
Be sure to tell the doctor that ordered your test if you are on Coumadin or other blood thinners. You will need special instructions.
The day before your test:
1. You may eat your normal breakfast. Do not eat solid food after noon.
2. Drink only clear liquids for lunch and dinner. These include:
water
apple juice
white grape juice
black coffee
tea
lemon or lime Jell-O
chicken or beef broth
lemon or lime Kool-Aid
soda pops, including colas, 7-Up, Sprite or Fresca
You should have at least one (1) to two (2) quarts of fluid at midday, another one (1) to two (2) quarts of fluid in the evening and again one (1) hour before bedtime. You should drink as much fluid as possible, with a goal of one (1) to two (2) gallons on the day you drink the laxative.
Do not drink red, orange or purple liquids, including Jell-O.
3. In order for the doctor to see the lining of your colon, it must be free from stool. You will have to drink Kleen-Prep Laxative solution to clean out your bowel. Be sure to use Kleen-Prep Laxative, NOT an enema product. You should plan to take the laxative in four (4) separate doses approximately six (6) hours apart. We suggest you begin the first laxative dose at 2 p.m. to allow the effects of the prep to be completed by bedtime.
Kleen-Prep is available with a prescription at your pharmacy. If you cannot tolerate this prep, an alternative is available by prescription. This alternative is called P.E.G. solution (trade names Nulytely, Golytely, Colyte) and is a very large volume. You will need to ask the doctor that ordered the test for a prescription for the P.E.G. prep.
Fleet Phospho-Soda Oral Saline Laxative instructions with suggestions for laxative times.
At 2 p.m., mix one-and-one-half ounces of Fleet Phospho-Soda Oral Saline Laxative, a sodium phosphate laxative a with four ounces of water or diet soda and drink immediately. You may be able to drink the solution faster by using a straw. Have another clear liquid immediately available to “wash away” the laxative taste.
At 8 p.m., mix one-and-one-half ounces of Fleet Phospho-Soda Oral Saline Laxative with four
ounces of water or soda and drink immediately.
Plan on being near a bathroom for the rest of the evening. Your bowels may begin to move in about 30-60 minutes. Feelings of nausea and bloating are common and resolve with time.
An A&D type ointment applied to the rectal area can help with any irritation. The goal is for your stool to be clear or light yellow water. Drinking at least a gallon of clear liquids during the evening will improve the quality of bowel cleansing.
4. Special instructions for P.E.G. preparation
If you have had a heart attack or heart failure in the past six (6) months, or have liver or kidney disease, you will need to use the P.E.G. preparation. Ask the doctor who ordered the test for a prescription.
The day of the test–important information
1. If you are unable to keep your appointment, please call the Medical Procedures Unit at(1) 328 8777, option 1 as soon as possible.
2. You may drink liquids, such as water or black coffee, up to two (2) hours prior to your colonoscopy. If you are also scheduled for an upper endoscopy, you should have nothing to drink for three (3) hours prior to your appointment time.
3. You should take your usual morning medications other than those noted earlier. This is especially important for anti-hypertensive and heart medications. You may take pain medication with a few sips of water up to four (4) hours before the test.
4. Please bring the following when you come for your colonoscopy:
A list of all medications you are taking
A list of any allergies you have
Health insurance cards
Your hospital card if you have one
A responsible adult to accompany you from the medical Procedures Unit after your procedure. You will not be discharged until that person is here to take you from the Medical Procedures Unit.
5. Please leave jewelry at home.
6. Small children will be more comfortable at home.
7. If you have diabetes, you should request an early morning appointment. If you take oral diabetes medications (pills): Do not take it the morning of your test. Bring it with you. If you take insulin (one (1) or two (2) injections per day): Take one half of your usual dose of NPH, Lente or Novolin 70/30 or Lantus insulin and NO Regular or Humalog insulin the morning of your test. If you take evening insulin, follow these same instructions for your dose the evening before your test. If you take Ultralente insulin or are on three (3) or more injections per day, please contact the health care provider who manages your diabetes.
The procedure
In the preparation/reception area you will answer questions about your health history, current medicines and allergies. You will sign a consent form.
After you change into a hospital gown, a nurse will start an intravenous line (IV). The IV will be used to give you medication to make you more comfortable during the procedure.
The procedure will be performed in a room specially designed for endoscopic procedures. Equipment that will help the nurse and doctor monitor your heartbeat and breathing will be connected to you.
You will be asked to lie on your left side. You will then be sedated before the doctor passes the lubricated tube into your rectum. As the tube passes through the curves of your colon, you may feel pressure or discomfort. You will receive medication throughout the procedure to keep you comfortable. The doctor will put air into your colon in order to see the lining.
You may have some bloating or abdominal discomfort from the air. You may feel as though you have to have a bowel movement. Pass the air if you feel the need. The doctor will remove as much air as possible after the procedure. If biopsy and/or polyp removal is necessary, you should experience no pain.
Potential complications
Complications are rare. However, there are potential complications associated with all medical procedures. These will be explained to you at the time you sign your consent for the procedure.
Your doctor
A doctor specially trained in gastrointestinal procedures will perform the test. The doctor who ordered your procedure will make decisions regarding your plan of care.
Recovery
After your procedure you will be taken to the recovery area in the Medical Procedures Unit. One family member may join you there. When you are ready to go home the nurse will discuss instructions and answer your questions. You will be given a copy of the procedure report. You may not drive yourself home. Be sure to bring a responsible adult licensed driver with you. A responsible adult will need to be with you when you are discharged from the recovery area. If your driver cannot accompany you for the entire procedure visit, please have them call(1) 328 8777, option 2 to confirm that they will be available when you are discharged.
At-home instructions
You will be given specific written instructions about resuming your medications and diet.
You may return to work or school the day after your test.
Do not drive a vehicle or operate machinery for at least 12 hours
after your test.
Do not make any major legal or financial decisions the day of your test.
Do not drink alcoholic beverages for at least 12 hours following your
procedure.
